Hi ,
I found this article on metal sensitivity and knee replacements

you may not be sensitive but your knee is on the detector . Depends how far you want to go . Sorry but I'm a registered nurse and could not help but put a clinical spin into this conversation .
Basic Science and Metal Sensitivity
All metals that come into contact with biologic systems undergo some degree of corrosion, and metal ions released from TKA components intra-articularly may form complexes with native proteins. These metal-protein complexes may act as antigens or allergens and cause an immunologic response in the body or synovial joint. The most common metal sensitizer in humans is nickel, followed by cobalt and chromium.4,5 Polyethylene and polymethyl methacrylate particles are relatively large and do not elicit the same response as metal ions.4,5
The prevalence of metal sensitivity in the general population is approximately 10% to 15%. Nickel sensitivity has the highest prevalence, approximately 14%, and cross-reactivity between nickel and cobalt is most common.5 However, the prevalence of metal sensitivity in patients with well-functioning implants, mostly of the hip, is approximately 25%.5 In a review of studies of patients with a failed, loose, or poorly functioning implant, the average prevalence of metal sensitivity was 60% (range, 13% to 71%).5 It is not known whether this phenomenon is a cause or an effect.
The pathophysiology of metal hypersensitivity to orthopaedic implants has been described previously in great detail.5 This implant-related hypersensitivity is generally a type IV allergic reaction, a delayed cell-mediated response, with activation of specific T lymphocytes. These and other lymphocyte populations release a variety of cytokines that perpetuate the inflammatory response and trigger the participation of activated macrophages.5 This response can produce substantial tissue inflammation and eventual periprosthetic tissue damage. Although it is known that Langerhans cells in the dermis are associated with skin hypersensitivity reactions, the particular cells in the periprosthetic knee joint responsible for the presentation of the metal-protein antigen are not known but could be endothelial cells, macrophages, or other synovial tissue cells.5
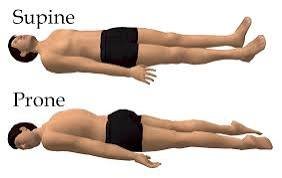
No generally accepted and reliable test is available for the clinical diagnosis of metal hypersensitivity to the components used in total hip arthroplasty or TKA.5 Dermatologists routinely have used a panel of cutaneous patch testing to different metal-salt complexes to determine hypersensitivity to a particular metal (Figure 1). An erythematous reaction to the allergen can be rated only qualitatively. However, controversy exists over the validity of patch testing to determine deep-tissue or joint hypersensitivity to metals.5 In a retrospective, case-controlled study of the sensitivity to metals in TKA components, Granchi et al6 reported on 94 patients who underwent dermal (back) patch testing to 11 metals and haptens for bone cements. In 20 patients who had no knee implant but who were candidates for TKA, 15% had positive patch testing to at least one metal hapten. Positive patch testing was significantly greater in a group of 27 patients with a stable knee arthroplasty (44%; P = 0.05) and in a group of 47 patients with a loose knee arthroplasty (57%; P = 0.001). No predictive value of the patch testing was seen in determining the fixation status of the TKA.6 The medical history for metal allergy identified by previous skin testing or a questionnaire was found to be a risk factor for the loosening of a TKA because failure was four times more likely in patients with prior symptoms of metal hypersensitivity.6
Figure 1
Figure 1
Clinical photograph demonstrating cutaneous patch testing on the upper back of a female patient who has persistent pain, synovitis, and stiffness after a total knee arthroplasty with an implant of a cobalt-chromium alloy. A mild allergic reaction to nickel, ...
Another test for metal hypersensitivity is the in vitro lymphocyte transformation test, in which peripheral blood lymphocytes from the patient are challenged with a variety of metal salts and the uptake of a radioactive nucleotide is quantified after 6 days.5 The final test is the in vitro leukocyte migration inhibition test, which quantifies the migration of cells in the presence of a sensitizing metal antigen by one of four methods.4,5 Few data show the utility of these in vitro tests for TKA patients, however. In a prospective study of 92 patients undergoing TKA in Japan, a modified lymphocyte stimulation test (mLST) was performed preoperatively, and 24 patients (26%) had a positive mLST response to at least one tested metal.7 The most frequent sensitizer was nickel, followed by chromium, cobalt, and iron.7 The clinical significance of these findings is unknown. At the present time, no evidence supports the routine or widespread preoperative patch or in vitro lymphocyte testing of patients for metal hypersensitivity before primary TKA.